Context:
Recently, the Comptroller and Auditor General of India (CAG) has highlighted irregularities in registration and validation of beneficiaries under the Ayushman Bharat – Pradhan Mantri Jan Aarogya Yojana (PMJAY).
More On news:

- In its audit report on Performance Audit of Ayushman Bharat, the CAG has revealed that nearly 7.5 lakh beneficiaries were linked with a single mobile number in the Beneficiary Identification System (BIS) of the scheme.
- Data analysis of the BIS database has revealed that there were large numbers of beneficiaries registered against the same or invalid mobile number.
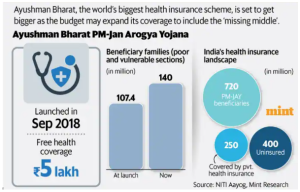
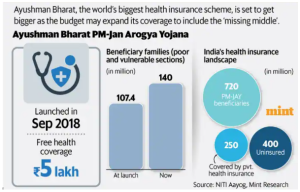
- AB-PMJAY is a Centrally Sponsored Scheme with some central sector components under Ayushman Bharat Mission anchored in the Ministry of Health and Family Welfare (MoHFW).
- It is an umbrella of two major health initiatives, namely Health and wellness Centres and National Health Protection Scheme:
- Health and wellness Centres: These centres provide comprehensive health care, including for non-communicable diseases and maternal and child health services.
- National Health Protection Mission (AB-PMJAY):
- AB-PMJAY provides a defined benefit cover of Rs. 5 lakh per family per year. This cover will take care of almost all secondary care and most of tertiary care procedures.
- To ensure that nobody is left out (especially women, children and elderly) there will be no cap on family size and age in the scheme.
- The benefit cover will include pre and post-hospitalisation expenses.
- All pre-existing conditions will be covered from day one of the policy.
- A defined transport allowance per hospitalization will be paid to the beneficiary.
- Benefits of the scheme are portable across the country and a beneficiary covered under the scheme will be allowed to take cashless benefits from any public/private empanelled hospitals across the country.
- Beneficiaries: The families covered under this scheme have been included on the basis of occupational criteria of Socio-Economic Caste Census 2011(SECC 2011).
- PM-JAY also included the beneficiaries of the then existing Rashtriya Swasthya Bima Yojana, which were not present in the SECC 2011 database.
- India is grappling with a “triple burden of disease” comprising persistent communicable diseases, a growing prevalence of non-communicable diseases, and injuries.
- There are challenges for India’s healthcare system to serve its 1.4 billion citizens adequately.
- The private sector handles around 70% of healthcare needs, but private providers are typically small, unregulated, and concentrated in urban areas, leaving underprivileged populations without proper care.
- Public hospitals are overwhelmed and hindered by insufficient funding, a lack of skilled health professionals, inconsistent drug and equipment supplies, and often overcrowding with more patients than they can handle.
- A significant factor contributing to these issues is India’s ongoing underinvestment in public healthcare, with government spending on health remaining at approximately 2.1% of the Gross Domestic Product (GDP).
- As a result, out-of-pocket expenses (OOPE)make up 62% of India’s total healthcare expenditure, exacerbating poverty and forcing nearly 60 million Indians back into poverty annually.
- Earlier government-funded health insurance schemes, such as Rashtriya Swasthya Bima Yojna (RSBY), targeted secondary care hospitalization but overlooked primary healthcare.
- Reachability: As of March 2023, more than 21 crore Ayushman Bharat (AB) cards have been created, and 28,561 hospitals are empanelled under PM-JAY in India, and the total amount incurred under PM-JAY is INR 53,942.7 crores.
- Role of Private Hospital: In the year 2022-23, approximately 56 per cent of the total admissions (in terms of amount) were authorised in private hospitals, while 44 per cent were authorised in public hospitals.
- Gender equity: Around 49% of Ayushman Card recipients are women, and over 48 per cent of the total authorised hospital admissions under the AB PM-JAY scheme have been availed by women.
- Inclusivity: The AB-PMJAY scheme added people from the transgender community to its list of beneficiaries.

- Beneficiary identification and registration: In the absence of adequate validation controls, errors were noticed in beneficiary databases such as invalid names, unrealistic date of birth, duplicate PMJDY IDs, and unrealistic size of family in a household, etc.
- Dead Getting Treatment: Patients earlier shown as ‘died’ continued to avail treatment under the scheme.
- States that reported the maximum number of such cases are Chhattisgarh, Haryana, Jharkhand, Kerala and Madhya Pradesh.
- Infrastructural Issues: There is a shortage of infrastructure, equipment, doctors and the quality standards prescribed under PMJAY guidelines have not been conformed.
- Indulgence in malpractices: 12 hospitals in Jharkhand and one in Assam allegedly indulged in various malpractices such as illegal collection of money from beneficiaries, repeated submission of the same photograph for multiple claims, and non-disclosure of facts.
- Faulty IT System: The CAG audit revealed that the IT system (TMS) did not prevent any patient from getting admission in multiple hospitals during the same period of hospitalizations.
- Same patient could get admission in multiple hospitals during the same period of hospitalization and there was no mechanism to prevent it.
- OOPE: PMJAY beneficiaries had to pay out-of-pocket for treatment (OOPE) under the scheme.
- Ex: In Himachal Pradesh, 50 beneficiaries of five hospitals had to manage their diagnostic tests from another hospital or diagnostic centre, and the cost was borne by the beneficiaries.
- Post Hospitalisation Cost: PMJAY is a hospitalisation scheme; leaving uncovered most out-patient treatment, including the cost of diagnosis and medicines.
- Poor follow-up actions: Actions like recovery of the amount of money collected, imposition of penalty, action against errant medical and paramedical professionals, de-empanelment of hospitals has not been initiated in most of the cases.
- Delayed in excluding ineligible beneficiaries: The report observes that delayed action in weeding out ineligible beneficiaries had resulted in ineligible people availing of benefits, and excess premium payment to insurance companies.
- Lack of speciality services: Lack of speciality services in many states forcing beneficiaries to move to far-off places causing hardship and inconvenience to them leading to OOPE.
- Skewed awareness pattern: Awareness of the benefits of the Ayushman Bharat scheme is higher among the rural beneficiary families in the southern region.
- Share of hospital admission is found to be higher in the Southern states such as Tamil Nadu and Kerala, viz 19.5% and 10.9%, respectively.
- Disproportionate AB card creation and hospital admissions: Highly populous states like Bihar and Maharashtra have very low percentages of AB card creation as well as hospital admissions.
- In spite of having a higher share of AB cards in the states of Uttar Pradesh and Madhya Pradesh, the hospital admission shares are low – 4.4% and 5.7%, respectively.
- Absent Grievance Redressal Systems: Out of 37,903 grievances, only 3,718 complaints (9.80 per cent) were redressed within turn – around-time while 33,100 complaints (87.33 per cent) were redressed beyond turn-around time.
- Stepping up enrollment: In order to realise the scheme’s full potential, the National Health Authority (NHA) along with its counterparts in the states should aim to provide every possible beneficiary with an Ayushman Card.
- Till 30 June 2023, the scheme has only enrolled 23,88,07,318 beneficiaries which aims to cover 50 crore people.
National Health Authority (NHA):
|
- Upgradation of the speciality services: There is a strong need to upgrade the speciality services of empanelled hospitals so as to fulfill the objective of the scheme.
- Incentivising Prevention: It should be made financially viable for a hospital for offering medication and lifestyle counselling to people.
- Following global budget model: Under this, the hospital is paid the premium for its enrolled patients at the start of the financial year which have a stake in preventing chronic health conditions from snowballing into catastrophic health expenditures.
- Multipronged Approach: Examining healthcare expenditure across various categories and cost savings through preventive care, improved regulation of drug prices, addressing insurance gaps for the middle-income group in India, collaboration with the private sector are essential.
Post Views: 190
